Pregnancy & Postpartum
Factors Essential For Healthy Pregnancy
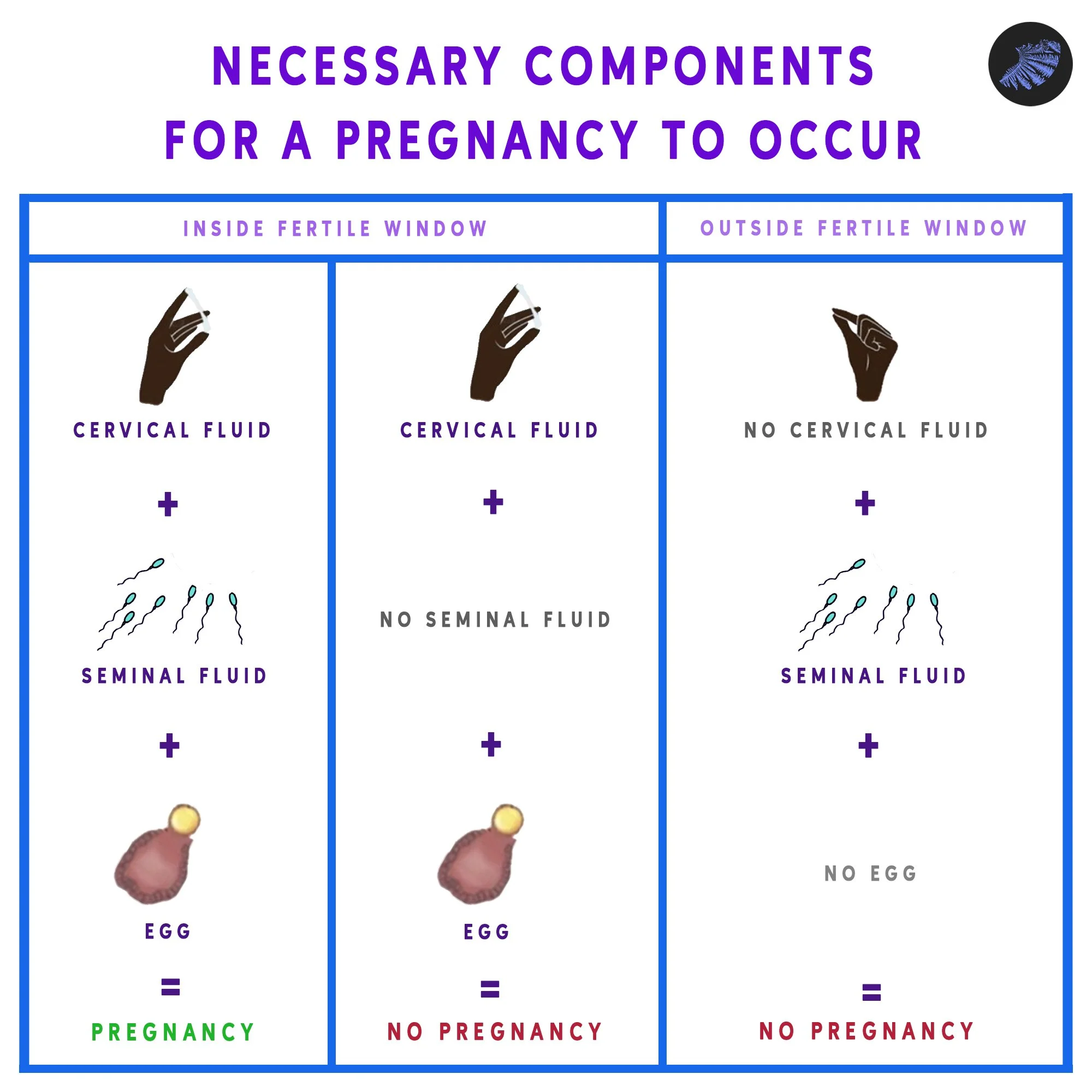
Unassisted Conception Occurs When These Components Are Present:
a chromosomally normal spermatozoon
a chromosomally normal egg
fertile quality cervical fluid
healthy patent (open) tubes in both people
typical sexual functioning during the fertile time
successful fertilization in the uterine tube
successful implantation in a healthy endometrium
healthy pregnant body and the ability to carry the pregnancy
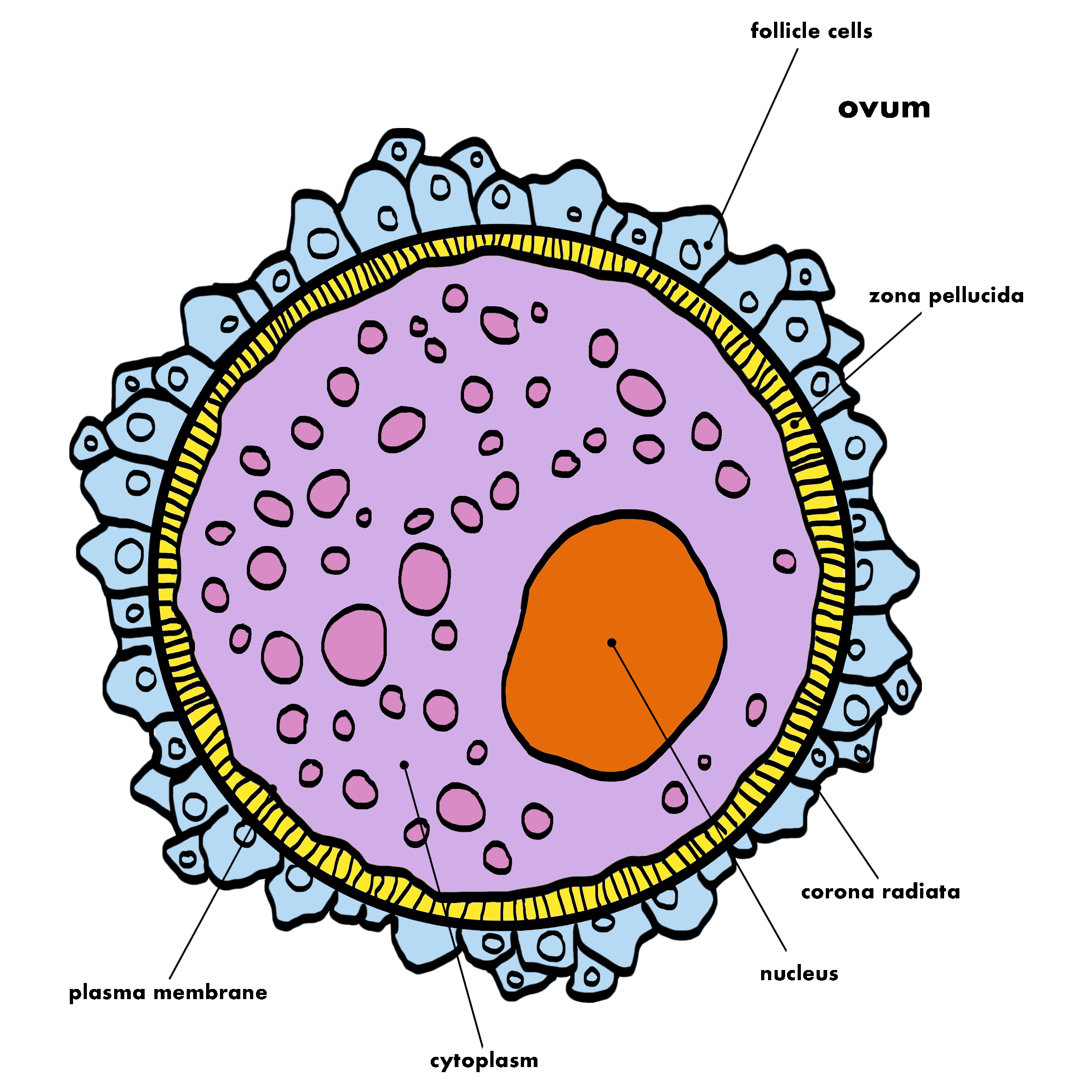
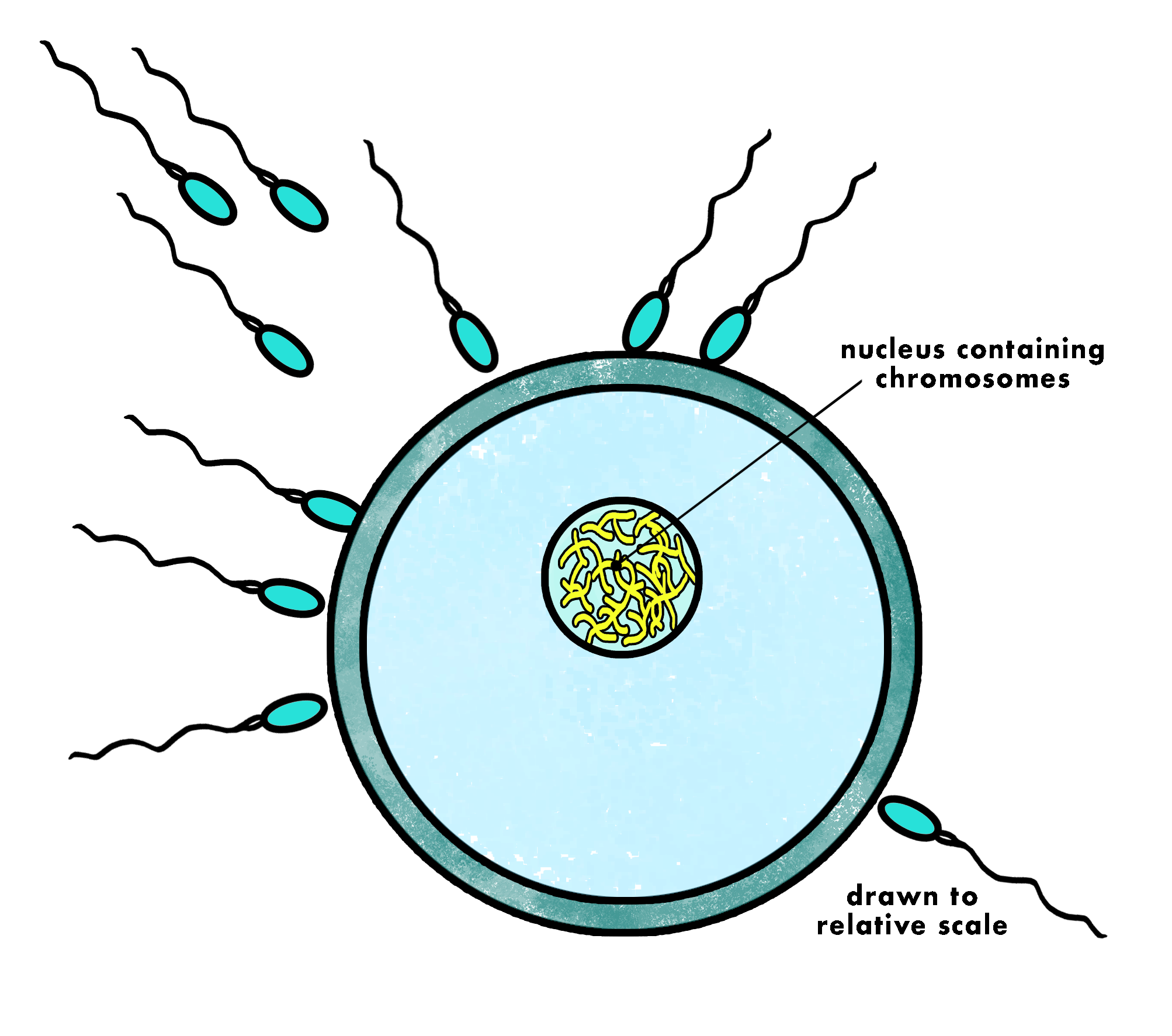
Ovum
The human ovum, also known as the egg or oocyte, is one of the largest cells in the human body, visible to the naked eye without the aid of a magnification device.
The ovum contains the female reproductive cell or gamete which is a crucial component in reproduction. Ova are produced and released once per cycle by the ovaries during ovulation.
The ovum is a single, large cell compared to the much smaller sperm cells. It is spherical in shape and consists of a nucleus, which contains the mother's genetic material (23 chromosomes), surrounded by a cytoplasm rich in nutrients to support early embryonic development.
To learn about each of the components of the ovum, visit our resource dictionary.
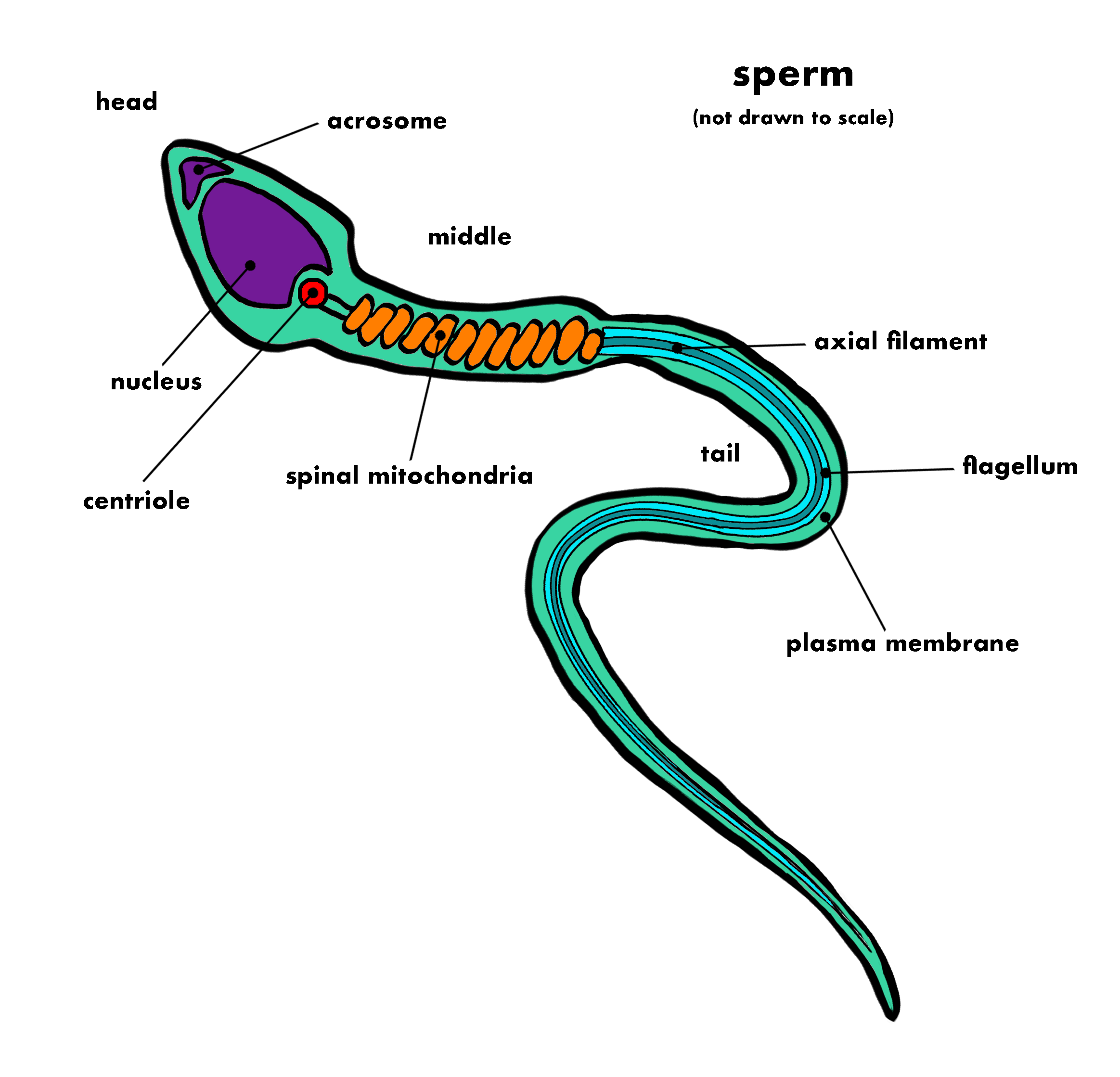
Human sperm represents the male reproductive cell or gamete.
Sperm are generated constantly throughout the lifespan and are stored in the epididymis. They are then released from the penis during ejaculation in a fluid known as semen. On average, each ejaculation may release nearly 100 million sperm.
Sperm are much smaller than the egg, and are selected carefully by the cervical fluid. Only about 200 will reach the egg, with only one sperm being selected.
Sperm cells consistent of a head which contains the nucleus and the genetic material (23 chromosomes), as well as the tail or flagellum, which allows for it to move. The head of the sperm is covered by the acrosome, a cap-like structure which contains enzymes that aid in penetrating the protective layers surrounding the ovum.
Sperm cells have a longer lifespan than the ovum, typically surviving in the cervix in the presence of cervical fluid for up to 5 days. This extended lifespan is why fertility awareness methods use the principle of the fertile window, and not just ovulation, to determine fertility. When ovulation occurs, a specific type of cervical fluid is released which allows for sperm that have been in waiting to continue upwards toward the potential ovum.
To learn about each of the components of sperm, visit our resource dictionary.
Sperm
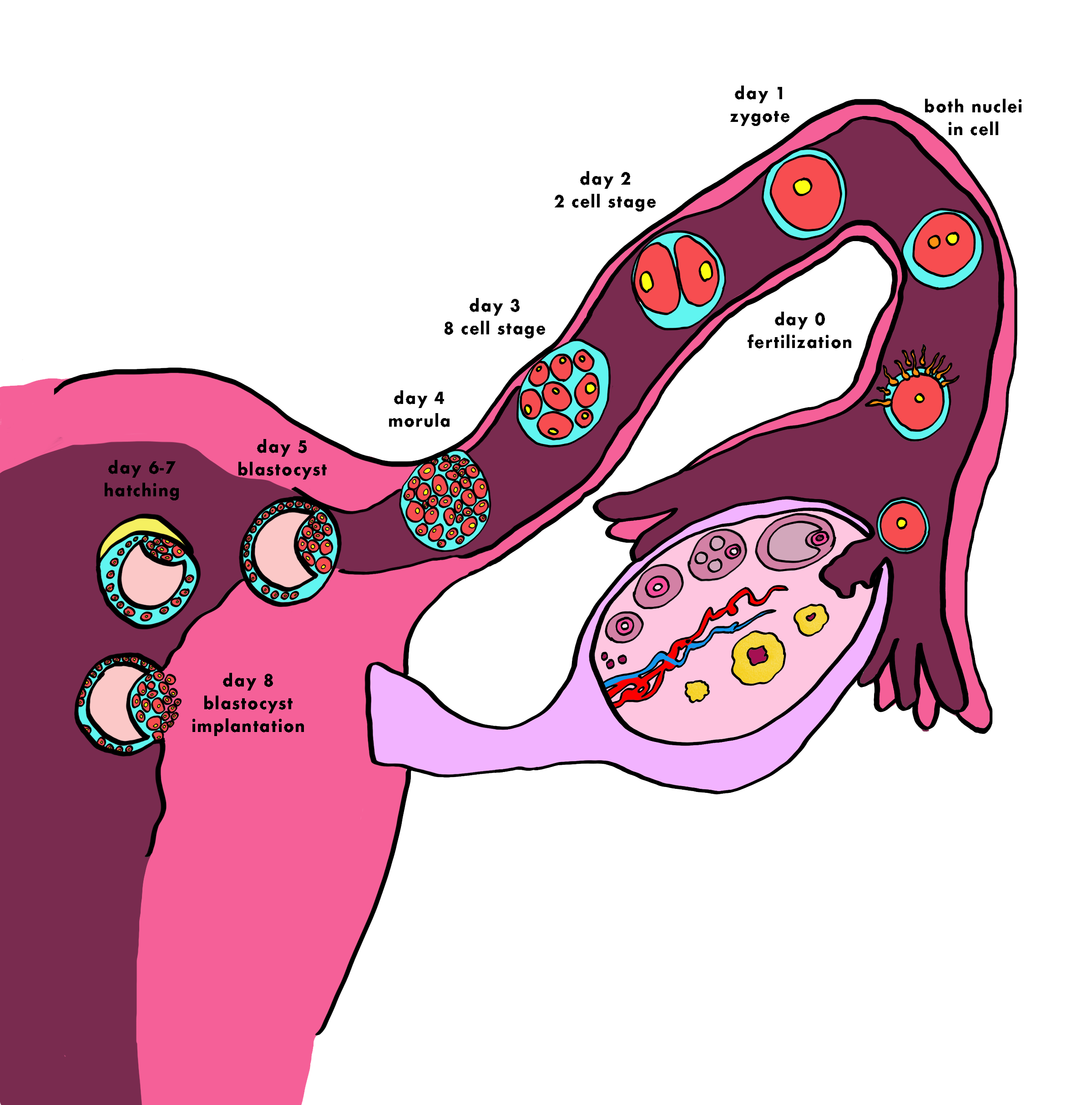
Fertilization
Once released from the ovary, the ovum travels through the uterine tube, where it may encounter sperm cells.
A fraction of the ~100 million total ejaculated sperm are selected by cervical fluid and transported through the cervix.
Human ova then release chemicals called chemoattractants that attract sperm to unfertilized eggs. The egg even knows how to distinguish and exhibit preference for different sexual partners regarding genetic compatibility.
On average, only 250 sperm make their way up the uterine tube to the site of fertilization.
Of these 250 remaining sperm, roughly 25 are capacitated, a biochemical process required for sperm to engage with the egg, and only these sperm are capable of responding to chemoattractants and fertilizing the egg.
Fertilization occurs when a sperm cell successfully penetrates and fuses with the ovum, combining their genetic material to form a zygote. The sperm enters the cytoplasm of the oocyte and the tail and the outer coating of the sperm disintegrate. The cortical reaction takes place, preventing other sperm from fertilizing the same egg. The sperm nucleus then fuses with the ovum, enabling fusion of their genetic material.
Implantation
The cells of the human endometrium (uterine lining) create a densely packed wall of cells that the fertilized egg must burrow through. It must implant and find a blood source to provide it with the energy it needs to grow. This process is called implantation, and is necessary for a healthy pregnancy to continue.
There are a few stages to implantation:
Cleavage: After fertilization, the zygote undergoes rapid cell divisions without significant growth, forming a cluster of cells called a morula. This process, known as cleavage, occurs as the zygote travels through the fallopian tube toward the uterus.
Blastocyst Formation: As the cleavage continues, the morula develops into a blastocyst, a hollow ball of cells with an inner cell mass and an outer layer called the trophoblast. The trophoblast will play a crucial role in the subsequent implantation process. Hatching refers to the event when the trophoblast cells break out of the protective zona pellucida, a thick glycoprotein shell that surrounded the blastocyst. The hatching process allows the trophoblast to make direct contact with the endometrial tissue, which is necessary for successful implantation. The exact timing of hatching can vary, but it generally occurs around 6-10 days after fertilization.
Implantation: Once hatching is complete, the trophoblast continues its interaction with the endometrial lining, facilitating the subsequent burrowing and attachment of the blastocyst to the uterine wall that involves releasing enzymes to facilitate the process.. This occurs about 5-7 days after fertilization, when the blastocyst reaches the uterus. After successful implantation, the trophoblast will develop into the placenta, and the inner cell mass will form the embryo, and the pregnancy commences.
hCG: After implantation, human chorionic gonadotropin, or hCG is released by an implanted embryo to support further development. Healthier embryos produce more hCG, and less healthy embryos produce less hCG. If not enough hCG is present, menstruation will occur. This is normal and happens to about a quarter of all fertilized eggs.
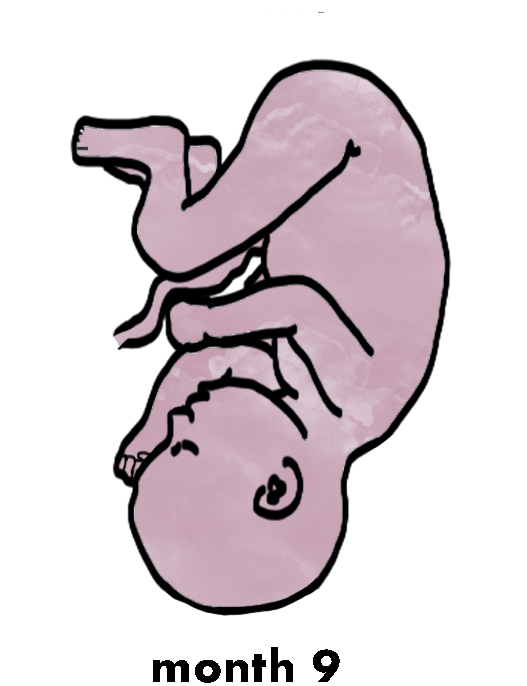
Fetal Development
A full term pregnancy is 40 weeks or 280 days. This time is divided into three stages, called trimesters. Each trimester is about three months.
1st Trimester: the fertilized egg will develop from a small grouping of cells to a fetus. The embryo at this time is only about ⅙ of an inch long, tadpole looking, and has a head and a trunk. Limb buds begin to appear that will develop into arms and legs. The tail-like structure will disappear and become a part of the tailbone by around 2 months.
2nd Trimester: The placenta is fully developed and the fetus can be felt moving around. The fetus continues to mature and develop reserves of body fat. The vernix caseosa begins to appear on the fetus to protect the thin fetal skin. This is also a time of rapid growth for fetal size and weight. Hair begins to grow, and the skin is wrinkly and red and covered with soft, downy hair called lanugo.
3rd Trimester: During the third trimester, the fetus is about 2 lbs and about 15 inches long. The brain develops rapidly, and the fetus can see and hear. Most internal systems are well developed but the lungs may still be immature. The fetus takes up most of the amniotic sac, continuing to gain more weight and making it more difficult for them to move. The fetus’s position may have changed to prepare for birth. Most often, they are head down in the uterus by month 9.
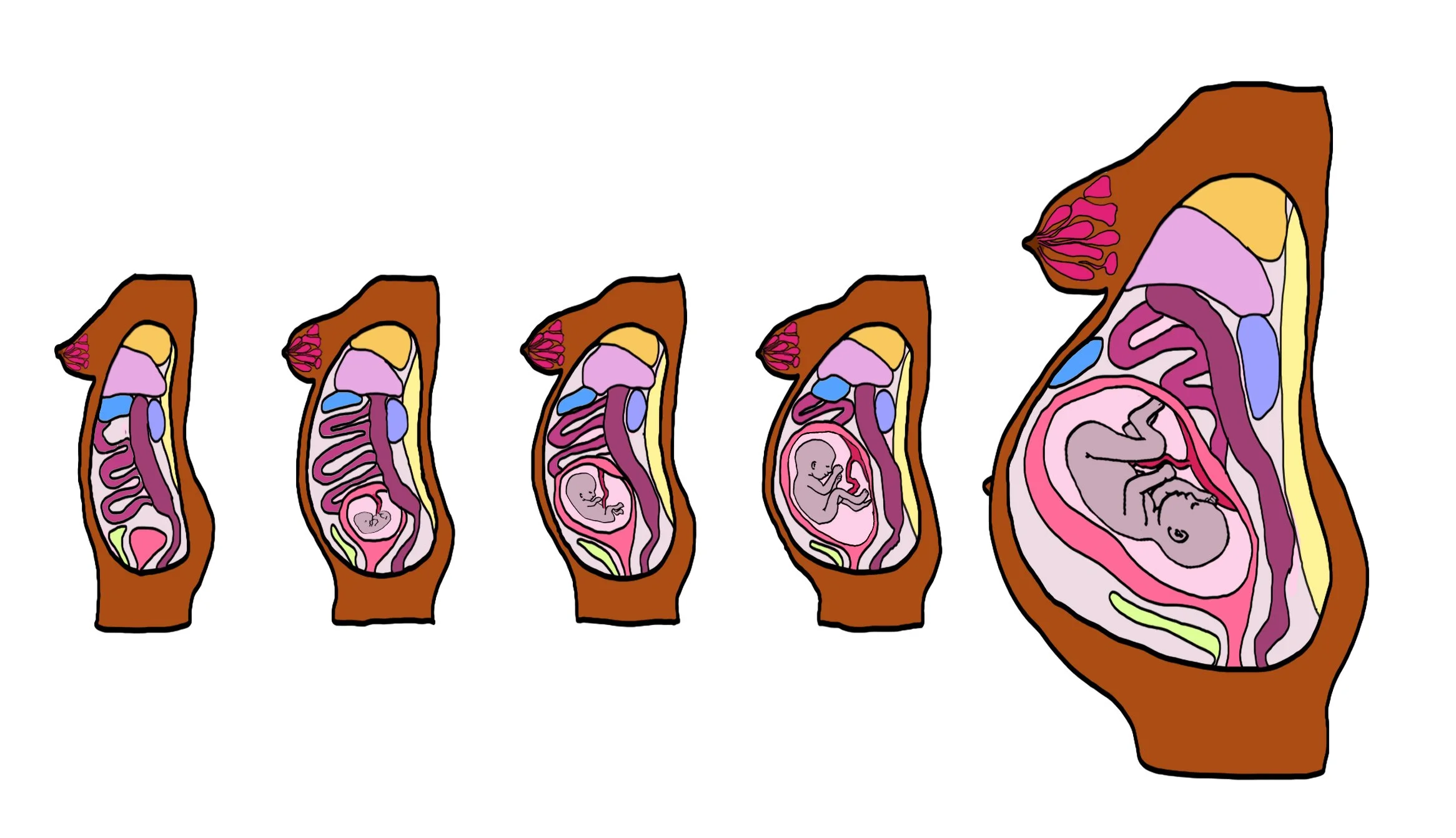
The Pregnant Body
breast development
During pregnancy, the breast undergoes both physical and functional changes to prepare for lactation. During the first trimester, high levels of estrogen instruct the ductal system to expand and branch out into the adipose tissue, decreasing the adipose tissue and resulting in ductal elongation. Prolactin is also stimulated by estrogen.
By mid-pregnancy, mammary glands are sufficiently developed to produce components of milk due to prolactin stimulation. Milk production is inhibited by high estrogen and progesterone levels, and colostrum is produced during this time.
In the third trimester and then rapidly after birth,hormone levels decrease, allowing for milk production and breastfeeding to commence. The areola may darken, the breast will increase in size, and the glands are more prominent.
organ shifting
In the first image we see the body pre-pregnancy or in the first stages of pregnancy, where the embryo is so small that none of the organs face disruption. Pregnancy has an impact on the organs inside the pregnant body.
Around 9-12 weeks the uterus is pushing the intestines together to make space.
By mid-pregnancy the stomach has swung upward by almost 45 degrees to sit close to the intestines.
By the third trimester, the organs are totally shifted, the liver and lungs get squeezed by your stomach and intestines, both of which used to be several inches lower.
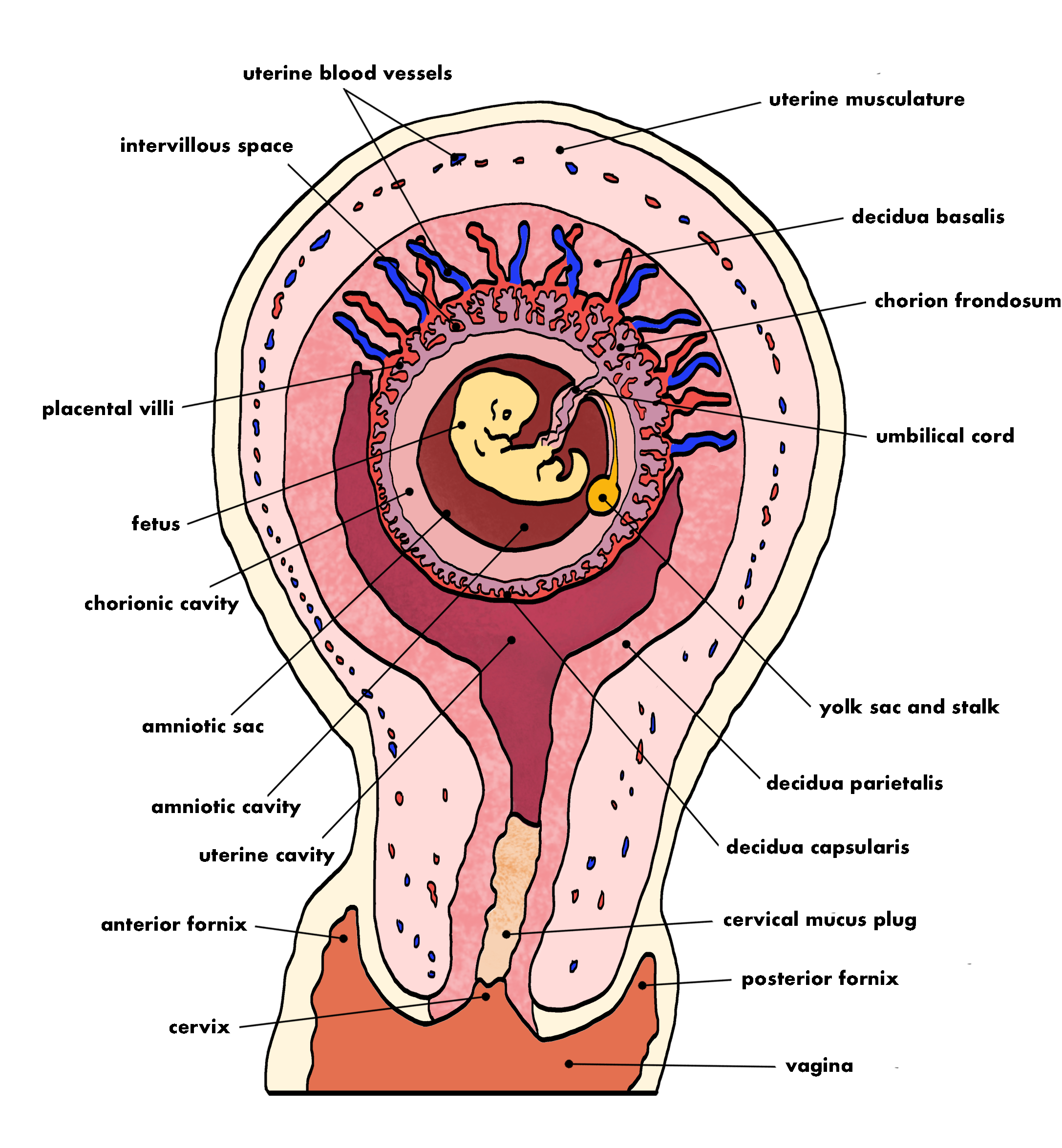
Placenta Development
Placenta development in humans is a crucial process that occurs during early pregnancy. After successful implantation of the blastocyst into the uterine lining, the trophoblast, the outer layer of the blastocyst, begins to undergo further transformation to form the placenta.
The placental villi roots in the endometrial tissue, creating finger-like projections called chorionic villi, which extend into the maternal blood-filled spaces called lacunae. The chorionic villi are responsible for facilitating nutrient and gas exchange between the maternal blood and the embryonic circulation.
As the placenta develops further, it acts as an interface between the mother and the fetus, providing essential nutrients, oxygen, and immune support to the growing embryo. The placenta also serves as a barrier, preventing harmful substances and pathogens from reaching the fetus. It is also responsive, and continues to grow and adapt to the increasing demands of the developing fetus. It is a temporary organ that is part of the endocrine system, releasing hormones, such as human chorionic gonadotropin (hCG), progesterone, and estrogen, which are crucial for maintaining the pregnancy and supporting fetal growth.
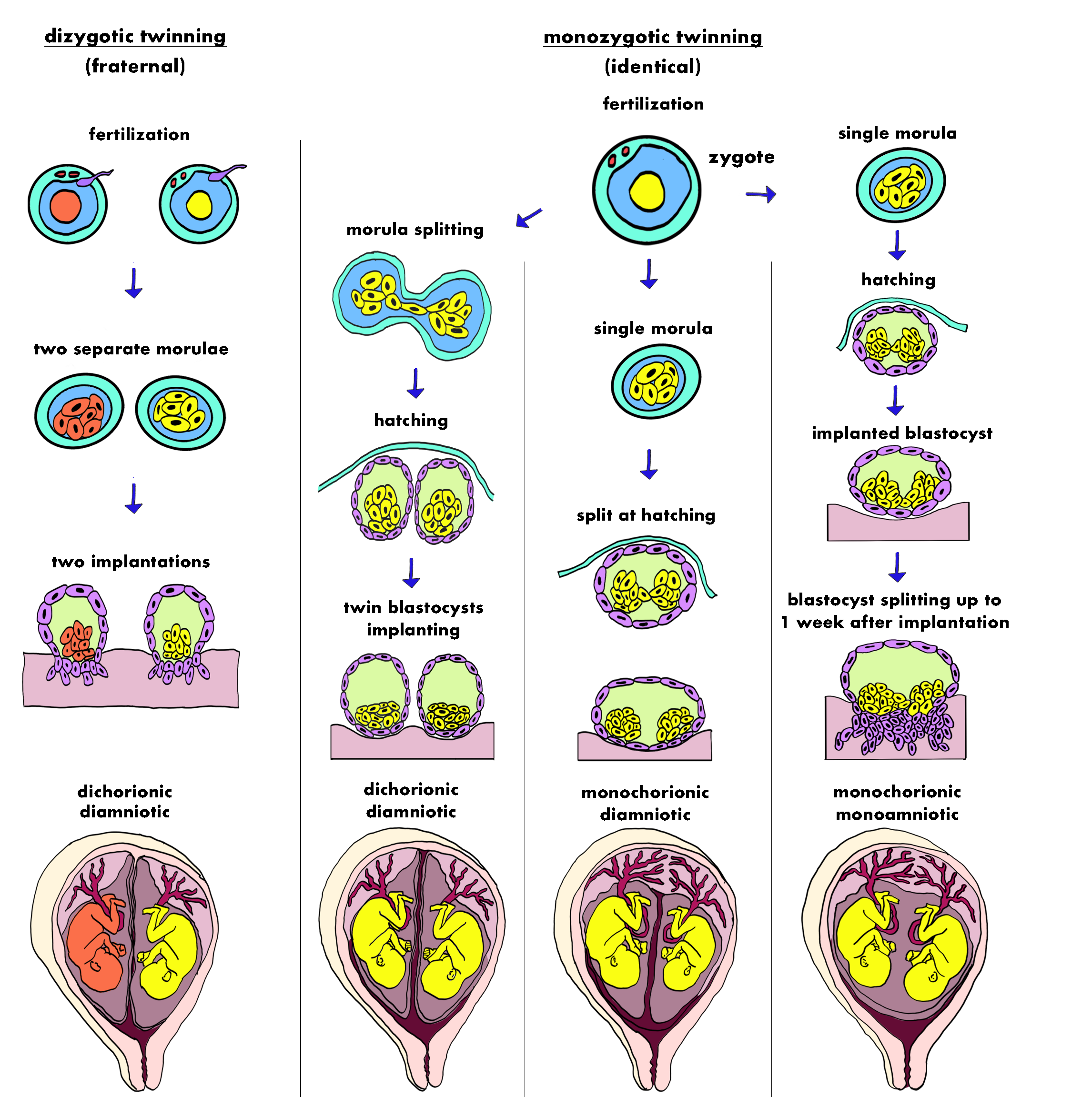
Twins / Multiples
Although single pregnancies are the most common, about 3% of the time, twins or multiples happen in pregnancy. This graphic helps us understand the different ways in which this can happen. The graphic is split into two scenarios, dizygotic twinning (fraternal) or monozygotic twinning (identical)
Dizygotic twinning - occurs at the first stage of fertilization, where two eggs were released instead of one. This is called hyperovulation and may be related to higher than average follicle stimulating hormone levels. This results in two separate morulae, which both implant into the uterus.
Monozygotic twinning - Identical twins result from the fertilization of a single egg by a single sperm, with the fertilized egg then splitting into two. Identical twins share the same genomes and are always the same sex.
Dichorionic diamniotic - the fertilized egg (zygote) splits at the earliest possible point of the morula stage. Hatching occurs separately and the blastocysts implant separately. This results in a dichorionic, diamniotic twin pregnancy, where identical twins do not share a placenta and each develops in their own separate amniotic sac.
Monochorionic diamniotic - the fertilized egg remains as one single morula, but instead splits during the hatching stage before implantation. When this happens, identical twins share a placenta but each develops in their own separate amniotic sac.
Monochorionic monoamniotic - the fertilized egg remains as one during the morula stage, and during the hatching and implantation stage, only splitting up to one week after implantation. This results in a twin pregnancy that is monochorionic and monoamniotic. In other words, these identical twins share a placenta and an amniotic sac.
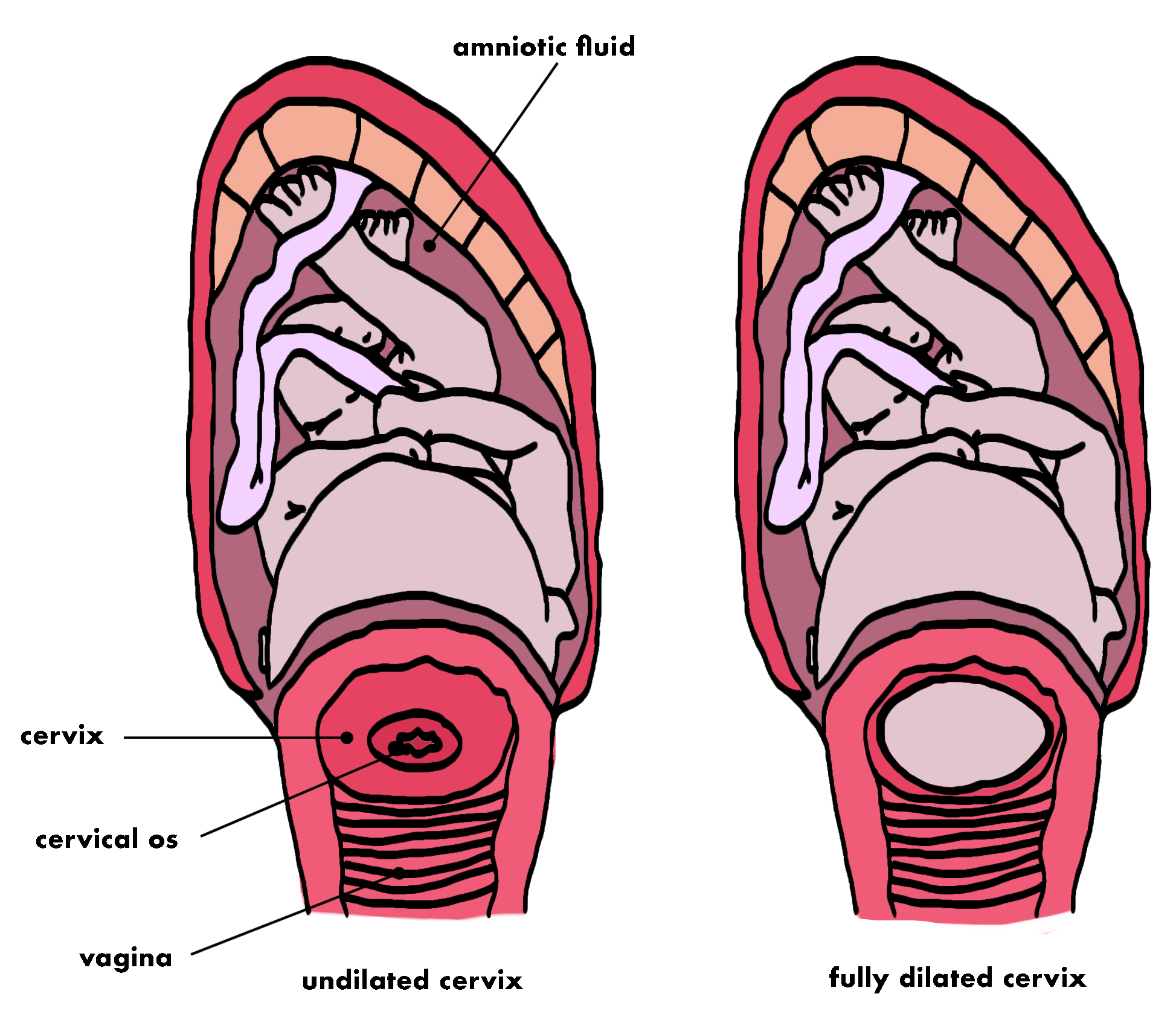
The Cervix in Labor
During labor, the cervix undergoes significant changes known as dilation and effacement to prepare for childbirth.
Cervical Dilation:
Cervical dilation refers to the opening or widening of the cervix, which is the narrow lower part of the uterus that connects to the vagina.
During the early stages of labor, the cervix is closed and tightly sealed. As labor progresses, contractions of the uterine muscles cause the cervix to gradually dilate and open up.
Cervical dilation is measured in centimeters and is typically described as progressing from 0 cm (closed cervix) to 10 cm (fully dilated). At 10 cm, the cervix is considered fully dilated, allowing the baby to pass through the birth canal.
Cervical Effacement:
Cervical effacement refers to the thinning and shortening of the cervix as it prepares for childbirth.
In its natural state, the cervix is long and firm. Effacement occurs as the cervix becomes softer and stretches in response to the pressure of the baby's head against it.
Effacement is measured in percentage, ranging from 0% (thick cervix) to 100% (fully effaced). When the cervix is fully effaced, it is thin and soft, making it easier for the baby to pass through the birth canal.
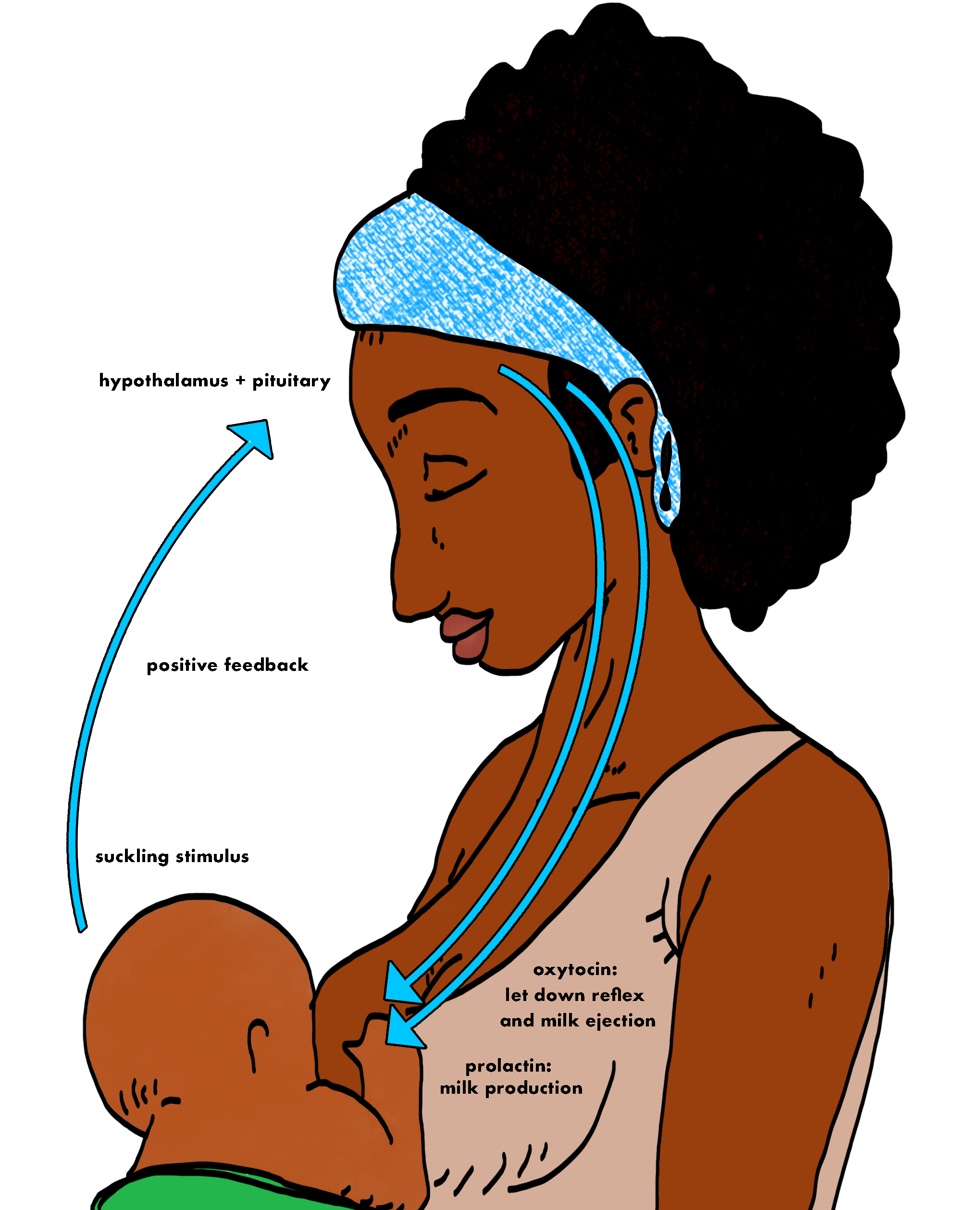
Breastfeeding
Breastfeeding is regulated by the hormonal interplay of prolactin and oxytocin. Prolactin triggers milk production in the mammary glands, ensuring a sufficient milk supply, while oxytocin facilitates the release of milk from the breasts during breastfeeding and fosters emotional bonding between the parent and baby.
Prolactin:
Prolactin is a hormone produced by the pituitary gland in the brain.
During pregnancy, rising levels of prolactin prepare the mammary glands in the breasts for milk production.
After childbirth, when the baby suckles at the breast, the act of breastfeeding stimulates the release of more prolactin.
Prolactin promotes the production of milk in the mammary glands, leading to an increased milk supply to meet the baby's needs.
The more frequently and effectively the baby feeds, the higher the prolactin levels, ensuring a steady and adequate milk supply for the baby's nourishment.
Oxytocin:
Oxytocin is another hormone produced by the pituitary gland, often referred to as the "love hormone" or "bonding hormone."
During breastfeeding, oxytocin is released in response to the baby's suckling and the stimulation of nerve endings in the nipples.
Oxytocin is responsible for stimulating the muscles surrounding the mammary glands, causing them to contract rhythmically.
These contractions help push the milk from the mammary glands through the milk ducts, allowing the baby to receive the milk effectively during breastfeeding.
Additionally, oxytocin plays a role in promoting bonding and emotional attachment between the mother and baby, enhancing the maternal-infant relationship.
<< Return to menstrual years
Next to perimenopause >>