Intro to PMDD
Premenstrual syndrome (PMS) is a common, recurrent condition affecting those who experience a menstrual cycle. It’s most often categorized by psychological and physical symptoms that occur during the luteal (post ovulatory) phase of the menstrual cycle.
Those with more severe symptoms are classified as having a related condition called PMDD, or premenstrual dysphoric disorder, a type of depressive disorder categorized by the Diagnostic and Statistical Manual of Mental Disorders.
75% of people who menstruate are affected by premenstrual symptoms, which includes physical and mental health effects, with around 8% of them experiencing severe pain and disruption.
3-8% of people who menstruate are diagnosed with PMDD, which is a condition focused mainly on mental health effects experienced in the second half of the cycle (luteal phase) leading up to menstruation, with physical effects being secondary.
Those who experience PMDD have a lower quality of life and functioning overall.
PMDD diagnostic criteria is outlined in the Diagnostic and Statistic Manual of Mental Disorders. In it, PMDD is a "depressive disorder not otherwise specified," emphasizing emotional and cognitive behavioral symptoms. The criteria states that
At least 5 of 11 symptoms (DRSP below) must be present for a diagnosis.
Symptoms should be limited to the post ovulatory, luteal phase
Symptoms should not amplify pre-existing depression, anxiety, or personality disorder
Symptoms should subside during the follicular phase of the menstrual cycle
These symptoms must present for two consecutive menstrual cycles
The symptoms include:
Markedly depressed mood, feelings of hopelessness, or self-deprecating thoughts
Marked anxiety, tension, feelings of being “keyed up” or “on edge”
Marked affective lability (e.g., feeling suddenly sad or tearful or increased sensitivity to rejection)
Persistent and marked anger or irritability or increased interpersonal conflicts
Decreased interest in usual activities (e.g., work, school, friends, hobbies)
Subjective sense of difficulty in concentrating
Lethargy, easy fatiguability, or marked lack of energy
Marked change in appetite, overeating, or specific food cravings
Hypersomnia or insomnia
A subjective sense of being overwhelmed or out of control
Other physical symptoms, such as breast tenderness or swelling, headaches, joint or muscle pain, a sensation of “bloating,” or weight gain
The Scientific Causes of PMDD
The evidence around PMDD is NOT conclusive.
However, there are a few things that we know about premenstrual mood conditions overall.
1. Premenstrual mood symptoms are the result of high histamine or mast cell activation. Mast cells are a type of immune cell that release prostaglandins, inflammatory cytokines, and histamine. Mast cell activation and the subsequent release of histamine cause symptoms that overlap with PMS including irritability, insomnia, breast tenderness, and migraines. Estrogen has two major peaks in the cycle, once before ovulation and once during the luteal phase (see below). Estrogen stimulates mast cells which release histamine and stops DAO enzymes from clearing histamine. Histamine also stimulates the ovaries to make more estrogen which can result in a feedback loop. Progesterone reduces histamine. This may link healthy estrogen metabolism and proper progesterone levels in the luteal phase to reducing PMS symptoms.
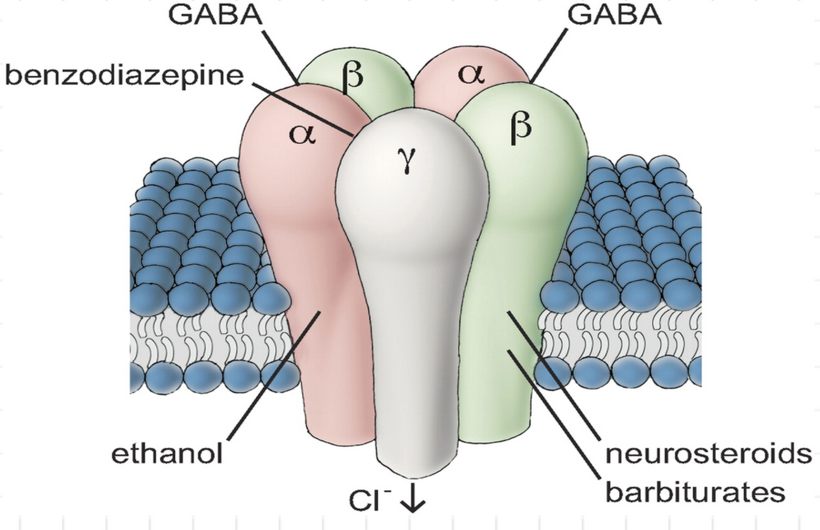
2. Premenstrual mood symptoms are the result of neurosteroid change sensitivity, or altered sensitivity of GABA receptors to allopregnanolone (the metabolite made from progesterone). This means those who suffer from PMDD have more sensitivity to the changes of progesterone that normally occur in the luteal phase. So it’ not that the menstrual cycle hormones are imbalanced, but that the body reacts in a more extreme way to the normal fluctuations. This altered sensitivity of the GABA receptors is considered a key physiological driver of PMDD symptoms and the behavioral effects of them. Typically progesterone has a positive effect on mood because its metabolite, allopregnanolone, calms GABA receptors in the brain. For some reason with PMDD, allopregnanolone in its normal levels can produce intense mood symptoms.
Gaba Receptor ^
3. Higher than normal levels of prolactin. Prolactin is a hormone made by the pituitary gland that causes the breasts to grow and make milk during pregnancy and after birth. Levels are normally low for non-pregnant people. Prolactin is also androgenic, because it increases the adrenal based androgen DHEAS. High prolactin has been linked to premenstrual mood symptoms.
4. Mineral deficiencies. Mineral deficiencies in magnesium, zinc, and b vitamins, especially b6, can cause severe menstrual mood issues. They help synthesize hormones, help manufacture brain neurotransmitters like GABA, dopamine, and serotonin, lower prolactin, promote anti-inflammatory compounds, help you metabolize estrogen properly, and lower histamine levels.
Contraceptive side effects are not PMS or PMDD
The progestins in birth control are not the same as the progesterone your body makes. In fact, progestins have many opposite effects, and are linked to anxiety and depression (whereas body made progesterone is linked with calm and happy moods). If you experience mood symptoms while using birth control, first, quit the birth control for at least three months before getting an assessment for PMS or PMDD.
Unfortunately one of the common conventional treatments for PMDD is to shut down ovulation and progesterone altogether with hormonal birth control, despite the lack of evidence supporting its usefulness for PMDD.
Determining the Difference Between PMS and PMDD
PMDD symptoms are severe and last for 7-14 days before menstruation
PMDD causes full episodes of uncontrollable emotion that damages relationships at work, home, and otherwise
PMDD causes those suffering from it to rearrange their lives to accommodate their condition
PMDD can manifest itself in extreme anxiety and suicidal thoughts
PMDD is focused on mental health changes whereas PMS is all encompassing of physical and mental changes before menstruation
Questions about the validity of PMDD as a separate condition remain
In 2000, the FDA approved four different drugs to treat PMDD, except the condition did not yet exist. Two years earlier in 1998, the FDA met privately with Eli Lilly, as their most famous antidepressant Prozac (fluoxetine) was about to expire. Eli Lilly determined independent of the American Psychiatric Association that PMDD was a distinct clinical disorder and that SSRI’s such as Prozac were effective treatments.
"The pharma industry went out trying to promote the condition so that more women self-presented with this disorder and consequently, put pressure on doctors to prescribe medications for them," said Saddichha Sahoo, MD, a psychiatrist at Ipswich Hospital in Brisbane, Australia, who wrote a paper about disease mongering in psychiatry, which included PMDD.
Eli Lilly changed the capsule color from green and yellow to pink and purple, and rebranded it Sarafem. Sarafem was FDA approved in 2002 and in the years immediately after, Zoloft (sertraline), Paxil (paroxetine) and the birth control pill Yaz (drospirenone/ethinyl estradiol) all won approvals for treating PMDD
Similarly, treatment guidelines to help doctors decide how to treat PMDD were issued before the condition was recognized as an official psychiatric disorder.
Typically such guidelines, which can be influential, are issued by medical societies or other groups. In this case, the 2006 guidelines were issued by a small group of researchers and were paid for by GlaxoSmithKline -- the maker of Paxil. The guidelines proclaimed antidepressants "the treatment of choice" for PMDD.
PMDD wouldn’t be declared a distinct psychiatric condition until 2013, when a panel of the American Psychiatric Association panel decided it was. However, 70% of the panel had direct ties to drug companies. By 2013, the demand had grown because of pharmaceutical sponsored marketing.
In contrast, Sarah Gehlert PHD ran a study in Illinois and Missouri and found that only 1.3% of premenopausal people have PMDD, so around 1 million in the USA, not the 6 million officially reported. "We did become convinced that some women had PMDD," Gehlert said, "but we could also see that it had the potential to harm women if it became a quick-and-dirty diagnosis."
“Over the past thirty years, clinical descriptions of PMS have remained predominantly psychological in focus, especially since the inclusion of premenstrual disorders in the American Psychiatric Association’s DSM (Diagnostic and Statistical Manual of mental disorders). First in the form of Late Luteal Phase Dysphoric Disorder (LLPDD) in 1987, and later its replacement, Premenstrual Dysphoric Disorder (PMDD), since 1994 (American Psychiatric Association 2000).
Even reputable clinical sources sometimes refer to PMDD as ‘severe PMS’; implying that PMS is simply a less severe form of a mental health disorder (for example, Lopez, Kaptein, and Helmerhorst 2012; Maharaj and Trevino 2015; Naheed et al. 2017). In comparison, thyroid conditions, which are also ‘hormonal’ in origin and commonly cause severe mood changes, are not listed in the DSM” said Sally King.
PMDD is a serious but rare condition
Only a small minority of people who menstruate fit the criteria for PMDD which requires medical support
The vast majority of people who menstruate can utilize the strategies above to treat their PMS successfully and improve their experience of menstruation by reducing menstrual related symptoms in just 3-6 months
PMDD is not to be used to argue that the menstrual cycle is a form of illness or that all people who experience a menstrual cycle are diseased and inferior
Recognizing our culture of menstrual stigma and countering the myth of the irrational female is important to distinguishing the way PMS is described and managed today